Osteoarthritis of the knee joint means a reduction in the performance of cartilage due to its curvature and destruction. Other terms are used to denote this disease -gonarthrosisideforming osteoarthritis. Currently, several methods of treating the disease are used: a certain option is selected taking into account the individual characteristics of the patient.
Specificity of the disease
Knee osteoarthritis usually develops progressively. It usually occurs in women and the elderly who are overweight or have venous defects. The disease can occur on one or both knees at once.
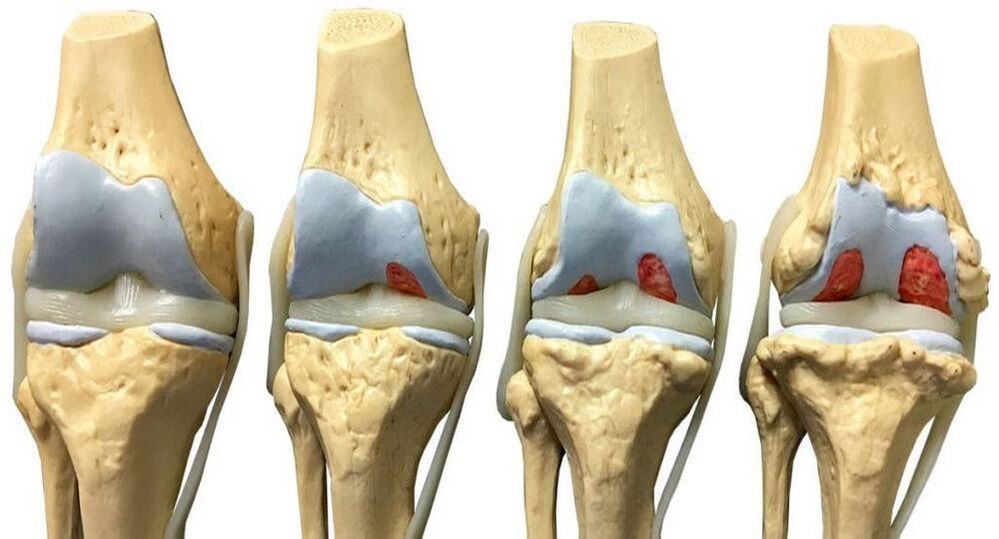
The main stages of development of knee osteoarthritis:
- Initial. There is a decrease in the amortization parameters of the joint due to the mutual friction of the cartilage and an increase in their roughness. Cracking is sometimes observed.
- Second. At this stage, the bone begins to be covered with growths (osteophytes). On the inner surface of the joint bag, the curvature is fixed, stiffness in the work of the extremities was noticed. As a result, the knee joint gradually reduces its functionality. Due to the decrease in the thickness of the intercartilaginous lining, a decrease in the distance between the tibia and the femur is observed.
- Third. If nothing is done, the pain in the knee area becomes permanent due to irreversible damage to the cartilage tissue. At this stage, the patient can no longer move normally.
The first symptoms of osteoarthritis of the knee joint are reason enough to consult a specialist. Otherwise, there is a real danger of disability.
Why osteoarthritis occurs
The main causes of osteoarthritis of the knee:
- hereditary predisposition;
- temporary immobility of the knee joint as a result of injury;
- surgical removal of the meniscus;
- high physical activity, constant hypothermia;
- obesity, overweight problems;
- ligament disorder (weakening);
- other joint diseases (arthritis, swelling, various inflammations);
- disorders of normal metabolism, lack of calcium in the body;
- flat feet (failure of the center of gravity increases the pressure on the wrist);
- stress, general fatigue, lack of sleep.
Symptoms
Signs of probable presence of osteoarthritis of the knee:
- Pain in the knee joint. The pain appears suddenly, in the background of physical exertion. In the first phase, we talk about an almost imperceptible lumbago, later the disease becomes more serious.
- Visual violation of the shape of the knee. This happens in later stages.
- Fluid accumulation, Baker's cyst. These are tangible seals in the back of the knee joint.
- The appearance of crunching cartilage, on the background of sharp pain. This indicates the second or third stage of gonarthrosis.
- Inflammation of the inner area of the joint sac. It is manifested by edema and increased cartilage.
- Knee stiffness due to severe pain, to complete immobilization. This happens in the advanced stages of the disease.
Treatment
Effective treatment of osteoarthritis of the knee joint is possible only with the use of an integrated approach. Modern medicine cannot yet offer one specific remedy that can eliminate this disorder. The success of treatment procedures depends on the timeliness of detection of the problem, which allows you to start the fight against gonarthrosis in the early stages.
Starting with treatment, the specialist pursues several goals:
- reduce pain symptoms as much as possible;
- to continue the normal flow of nutrients to the joint;
- increase the intensity of blood circulation in the knee area;
- restore the functionality of the supporting muscles in the problem area;
- make the knee as mobile as possible;
- expand the space between the joined bones.
The exact treatment algorithm is determined on an individual basis. Distinguish between conservative and surgical techniques.
conservative method
This approach is used in the early stages of the disease, and consists of the use of various drugs and therapeutic exercises.
Painkillers, anti-inflammatory drugs
To eliminate or reduce pain in the knee joint, the doctor usually prescribes the use of nonsteroidal anti-inflammatory drugs. They are presented in pharmacies with tablets, ointments and injections. Gels, ointments and patches for warming and anesthesia show good effectiveness in relieving pain.
A positive result in this case is usually achieved in 3-4 days. It should be understood that these drugs do not eliminate the disease, but only reduce the pain. It is recommended to take painkillers only on the advice of a specialist and only in the case of relieving unbearable pain. The fact is that the NSAIDs cause various side effects (especially the gastrointestinal tract).
Hormonal drugs
In some cases, your doctor may prescribe hormone injections to relieve the pain of osteoarthritis of the knee. This approach is used when the effectiveness of NSAIDs is weak in the background of progressive disease.
Hormones are prescribed for a short period (1-10 days) during exacerbations of osteoarthritis and accumulation of fluid in the knee joint.
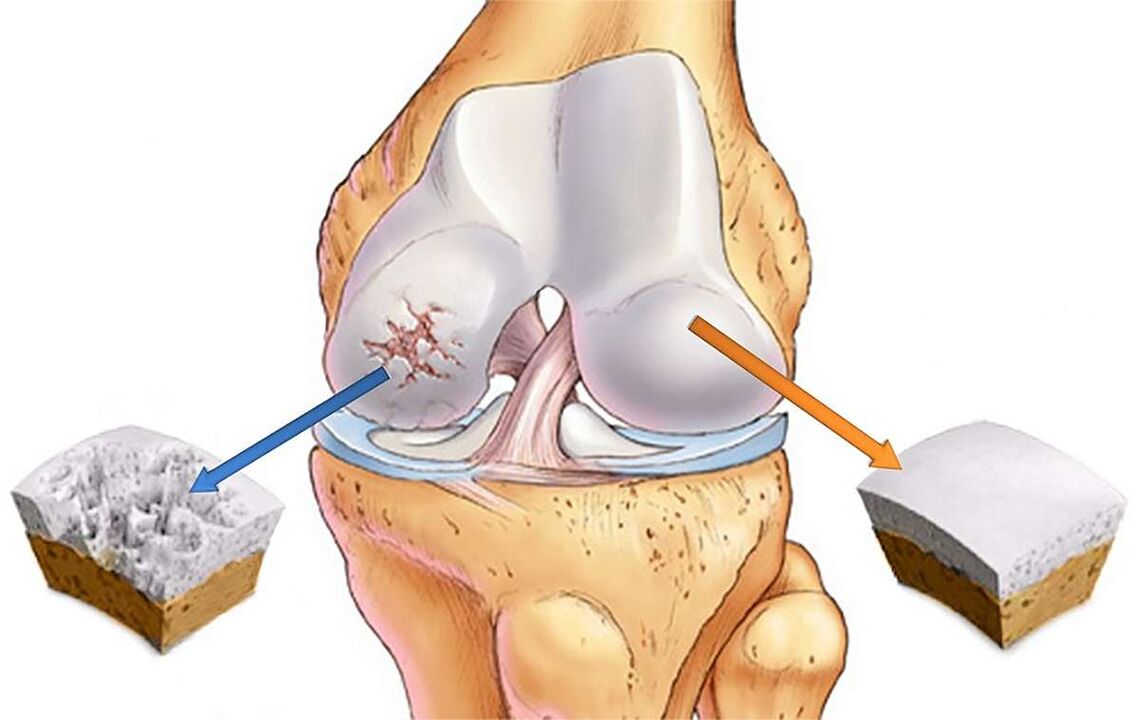
Chondroprotectors
For the renewal and nutrition of the cartilaginous layer at the beginning of the development of the disease, the so-calledchondroprotectors (glucosamine, chondroitin sulfate). Glucosamine starts the process of cartilage regeneration, corrects metabolism, blocks destructive processes. Chondroitin sulfate disarms dangerous enzymes, increases the amount of collagen (this protein nourishes cartilage with moisture). According to leading doctors, these drugs currently show the greatest positive effect in the treatment of gonarthrosis.
In particularly critical cases, when cartilage tissue has suffered serious anomalies, chondroprotectors are ineffective. When prescribing glucosamine and chondroin sulfate, the doctor states certain daily doses. Only a systematic approach to taking these drugs gives a chance for positive results. They are sold in tablets, capsules, injections, gels.
Vasodilators
To eliminate spasms of the vascular system, optimize blood flow and metabolism in the knee area, the doctor prescribes vasodilators. As a rule, they are prescribed in combination with chondroprotectors. If, on the background of osteoarthritis, the fluid in the knee does not collect, it is allowed to rub the joint with warming ointment and attend therapeutic massage sessions.
Hyaluronic acid
Due to its chemical composition, this substance is very close to intra-articular fluid. After entering the joint, the acid creates a film that protects the cartilage from friction with each other. The use of the drug is allowed after the cessation of exacerbation.
Therapeutic exercise
For knee osteoarthritis,resort to exercise, but only under the strict supervision of a doctor or an experienced trainer. Self-medication is strictly forbidden, given the huge risks of any careless movements and loads. Proper use of physiotherapy exercises helps keep the joints in working order, eliminates muscle cramps and alleviates unpleasant symptoms. It is strictly forbidden to engage in physiotherapy exercises during exacerbations or in inappropriate conditions.
Physiotherapy
Proper application of physiotherapy techniques can significantly reduce knee pain, relieve inflammation and improve the flow of nutrients to the joint tissue. Before prescribing physiotherapy, the orthopedist conducts a detailed diagnosis of the problem area, prescribes general and special tests, sends an ultrasound or X-ray. This approach allows you to get a real picture of the problem and choose the best methods.
The following types of physiotherapy have a good analgesic effect:
- UV radiation. Exposure to ultraviolet rays reduces the sensitivity of nerve endings and reduces pain. It is usually prescribed in the later stages of the disease. The standard duration of treatment is 7-8 sessions.
- Local magnetotherapy. Improves the overall health of the patient by reducing pain, inflammation, muscle cramps. Magnetotherapy is usually prescribed at the first fixation of knee osteoarthritis symptoms. The standard number of procedures is 20-25 sessions of 30 minutes each.
- Infrared laser therapy, UHF, SMW devices, ultrasound, therapeutic baths, etc.
If the disease has passed into the stage of dystrophic and deforming changes, the doctor recommends sanitary-sanitary treatment. A special list of procedures is compiled after careful study of the patient's history.

Operation
This approach, with proper application, can partially or completely restore the work of the knee joint. The formation of the algorithm of surgical intervention takes into account the degree of destruction of cartilage tissue, the degree of inflammation, the amount of fluid collected, etc. As a rule, surgical intervention is practiced in the late stages of gonarthrosis. This approach involves fragmentary or complete replacement of the affected joint with an endoprosthesis.
Main approaches to surgical treatment:
- Arthrodesis of the joint. During the operation, the surgeon fixes the leg in the most comfortable position for the patient, followed by immobilization of the knee joint. Defective cartilage is completely eliminated. Such a radical approach is relevant only in extreme cases.
- Arthroscopic debridement. It is used in the second stage of knee osteoarthritis development. Surgical removal of damaged cartilage tissue is performed, which allows you to save a person from pain for several years (usually 2-3 years).
- Endoprosthetics. In this case, the knee joint or its special part is replaced with a plastic, ceramic or metal implant that completely repeats the anatomical configuration of the natural joint. Endoprosthetics are today considered the most effective way to restore a full-fledged lifestyle to a knee patient with osteoarthritis in the next 15-20 years.
Competent planning and implementation of surgical treatment allows to improve the patient's well-being and restore his mobility (partially or completely). At the same time, it should be borne in mind that after the operation, a long period of recovery will be required, attending physiotherapy exercises, mechanotherapy, diet, etc.
Rehabilitation
On average, the rehabilitation period after surgical treatment lasts 90 days:
Main tasks of rehabilitation:
- restoring the patient's ability to move normally;
- optimization of muscle and joint function;
- creating a protective block for the prosthesis.
Drainage is removed 2-3 days after the operation, after which you can try to walk carefully. To relieve pain, the doctor prescribes medications with a cooling effect. Small symptoms of pain sometimes last for a year after surgery: this is due to the fact that the prosthesis takes time to heal. Elderly patients recover longer: nonsteroidal anti-inflammatory drugs are prescribed to alleviate the condition. In some situations, the doctor prescribes hormonal agents that have a pronounced effect.
One week later, the patient enters the rehabilitation center under the supervision of an experienced physiotherapist. The individual characteristics of the body are taken into account when designing a course of exercise therapy. Classes are held regularly (daily), with a gradual increase in load: this protects against injury and tissue rupture.
Period after discharge
Upon completion of the stay in the rehabilitation center, the patient is discharged, with detailed recommendations regarding his future lifestyle. Dancing and light gymnastics are allowed after 6 months from the date of surgery. As for serious loads (speed running, jumping, sports games, squats with heavy weights), they must be completely excluded. Otherwise, the prosthesis will fail quickly.
Do not lift heavy objects heavier than 25 kg. Inside the apartment it is necessary to place support handrails: they are placed on the stairs, in the shower and bathroom. All pieces of furniture must be fully functional (especially chairs). These and other measures will maximize the life of the prosthesis. You should also be prepared for postoperative osteoarthritis of the knee joint, which can last up to 3 years.
Disease prevention
The best way to deal with any disease is to prevent it from occurring.
Effective waysprevention of knee osteoarthritis:
- Proper nutrition, maintaining a normal weight. It is better to eliminate fatty and fried foods, alcohol, coffee, etc. from the diet. Experienced nutritionists can give detailed advice on this.
- Be careful when doing sports. It is desirable to reduce the load on the joints as much as possible.
- Be careful of all diseases (especially infectious), treat them properly and avoid chronic stages.
- Pay attention to posture, do not be negligent about diseases of the bones and spine.
- Include mild physical activity in your daily routine (cycling, swimming, walking, doing exercises to strengthen your joints).
- Avoid any self-medication options for knee arthritis. At the first symptoms of the disease, contact the clinic immediately.
- Lead a quiet lifestyle without stress and lack of sleep.
- Take measures to strengthen immunity (hardening, taking vitamins).
- Dress warmly in the cold season.
By applying the principles of a healthy lifestyle in your life and seeking medical help in a timely manner, you minimize the risks of developing osteoarthritis of the knee joints. When choosing a clinic, preference should be given to proven treatment centers equipped with modern equipment.



















